If you’re like most people, the referral for services is the first time you’ve ever heard of applied behavior analysis (ABA). The question then becomes, Now what? You do some research and find that that ABA is an effective treatment for autism. Next, you find a local ABA provider. But, since you’re still not 100% sure what they do, you’re not sure what questions to ask.
That’s what I’m here to help with. By talking to parents that I’ve worked with, I’ve managed to collect the top 10 questions parents wish they knew before starting services.
Before we get discuss those questions, though, here’s an overview of how the enrollment process works:
Check pre-authorization from insurance
An administrator will call your insurance to verify coverage for ABA services. ABA services are generally covered with an autism diagnosis. (~ 1-3 days)
Provide an initial assessment/screening
Depending on the provider, the initial assessment can range from 1-8 hours. Longer assessments will typically be a mixture of caregiver questionnaires and direct testing (sometimes in multiple environments). Also, longer assessments may be spread across a few days, since anything over 3-4 hours of testing can be overwhelming for a child. (~ 1-3 days)
Write a report with recommended hours
Based on the assessment, the BCBA will recommend hours if it is in their realm of expertise. For example, if your child may not need intensive one-on-one treatment but would benefit from a social skills group, you may see a referral to another BCBA who specializes in this area. Another example is if feeding is a behavioral issue for your child, you may be referred to a BCBA with more experience in feeding. (~ 3-5 days)
Submit report for authorization
Although the provider received pre-authorization for an assessment and services, authorization is required by most insurance companies before they will cover the cost for recommended hours. (~ 1-5 days)
Set up data collection for goals and train therapists for ongoing services
Once a provider receives authorization, the BCBA will create a protocol book for therapists to collect data and measure progress under each of the client’s goals. Training therapists is the step that parents have the most questions about because they don’t realize it is a team of therapists that will be providing treatment. We will touch this point again in the top 10. (~ 3-5 days)
Now that you know how the enrollment process works, here’s our Top 10 Questions that parents wish they knew to ask before starting ABA services. I’ve also provided some answers to give you more insight into ABA services and the process as a whole.
1. Who are the people providing therapy to my child?
ABA services are typically based off a tiered delivery of service. More information about this is documented in the consumer guidelines on the BACB website. Basically, you'll be working with 1 board certified behavior analyst (BCBA) and a team of registered behavior technicians (RBT or other qualified staff). The BCBA will assess and write your child's treatment plan and train therapists to implement the treatment plan. Because of the range of hours ABA requires (see question 2), the BCBA does not necessarily provide direct treatment on a daily basis. Your child's main interactions are with the RBTs covering the recommended hours. The BCBA collects information from the daily data to monitor progress, make modifications, and train when necessary. The BCBA is also responsible for parent trainings and care coordination (see question 9) with other therapies your child may be receiving.
2. How will hours vary per recommendation?
Parents are often surprised to hear that ABA can require up to 40 hours of therapy. Keep in mind, though, recommendations will vary based on the BCBA, setting, and your child's current skill sets.
The BCBA will assess your child's needs and use their clinical judgement (interpretation of the assessment) to recommend hours based on how the BCBA can address the areas of need.
Setting plays another factor into the recommended hours. Settings may include clinic, in-home or shadowing. Sometimes companies offer a mix of service (see question 4). From my experience, recommended hours are higher in clinics because they offer opportunities for peer play and group activities. Since therapists do not travel, it offers the opportunity for your child to easily transition between multiple therapists (approximately 2 or 3) throughout their day, which promotes generalization. In-home therapy tends to have a lower range of recommended hours because of the commute for therapists and accommodating therapist and client schedules. However, in-home therapy provides additional benefits that make up for the lower recommended hours, such as learning in the natural setting (living room, kitchen, bedroom, etc.) and higher family involvement.
Not all children are recommended the full 40 hours of therapy. Some of this is based off your child’s current skill sets. For example, if your child’s communication is on par with their peers, but they either can’t initiate or initiate inappropriately (e.g. pushes friends), then the amount of recommended hours may fall within the lower range.
As you can see, there are a variety of reasons for the number of hours a BCBA recommends. After an initial assessment, you should receive a breakdown of the goals that will be worked on within the weekly recommendation.
3. What are extinction bursts?
The BCBA will warn you that behaviors are going to get worse before they get better. ABA is based on patterns of learned behavior, meaning we examine events that surround the behavior you want to change. For example, if your child always throws tantrums at the grocery stores, there is something going on the at the grocery story that triggers, but also reinforces, the tantrums so that they happen again and again. The BCBA’s job is to figure out what the triggers are and what is reinforcing the tantrums. From there, the BCBA will put a stop to whatever is reinforcing the tantrums. However, the stop does not happen immediately. Your child is used to getting something in return to quiet down at the store, such as being held, full access to your phone, a straight shot to the gaming section, or you turn around and head home. It’s when your child doesn’t get this reward when the tantrum may get worse because they are upset at no longer receiving what they want.
4. Where does ABA therapy take place? Can I have a tour?
Setting will vary based on provider. Some providers exclusively offer in-home or clinic-based therapy, while some clinics are a combination of the two. There’s also a chance of shadowing opportunities at your child’s school or daycare, depending on if the provider is willing to shadow at the school and if the school agrees to allow an outside provider on campus. Sometimes, schools will provide their own shadows. Another possibility is a community outing to somewhere like a restaurant, park, or a grocery store, though, due to liability, providers are often cautious with these outings.
Remember to ask your provider about all options so you have a better idea what the best fit for your family and lifestyle is. If they are center-based, ask for a tour to observe the learning environment. It’ll put your mind more at ease.
5. Do you provide parent training?
Be sure to ask about parent training and how often it occurs. Some places will conduct parent trainings in groups, while some are one-on-one. Scheduling meetings is sometimes difficult because the BCBA is training staff, conducting sessions, and modifying treatment goals, but parent training is especially important because your child should be able generalize their skills to the home and community.
6. What does therapy look like?
Ask your ABA provider to describe or show you (at the tour) what ABA looks like. ABA can be done at the table or on the floor or almost anywhere. Some clinics will structure your child’s day with activities throughout the day. It’s also good to note how therapists are taking data because it is how we measure progress.
7. How long is the intake process?
As mentioned in our checklist, verifying insurance and authorization can take a while, especially if the provider is verifying benefits for multiple clients. With that aside, some other questions to ask would be:
a. How long is the assessment?
Assessments/screenings to qualify for services range from 1 hour to 8 hours, across multiple days. Again, it depends on the provider and the assessment tools they need to make a clinical decision on if they can help your child.
b. What is your staff availability?
Staff availability is typically tough because it comes down to working with multiple schedules. Schedules would be easier if sessions were one time per week, but since providers are trying to build approximately 6 – 40 hours per week (based off the recommendation), it may take some time to build your child’s team and fill the recommended hours.
On the flip side, staff availability may be abundant to due recent discharges, so your child may get to start sooner. It’s definitely a question to ask so you’re better prepared when your child starts therapy.
8. Will my child be receiving one-on-one therapy?
This question goes along with the structure of your child’s therapy. Some providers offer group instruction versus one-on-one therapy or they may have a combination. Your child may benefit more from group than one-one-one or vice versa depending on the results of the assessment.
Another question that goes along with this is, What happens when a therapist calls in sick or you need to cancel? The provider can answer questions about their policy and procedures.
9. Do you provide care coordination with other disciplines?
If your child is receiving other services such as speech or occupational therapy, ask if your provider communicates with other professions. If your child is in school, you might try reaching out to their teacher. Of course, you’ll need to sign a Release of Information form to comply with confidentiality standards.
Care coordination is important because if your child has interfering behaviors in their speech sessions, they may be making little progress towards their speech goals because they are working on behavior management. On the flip side, if your child is working on communication as a replacement behavior for aggression, the collaboration with a speech therapist is important to make sure the behavior analyst is effectively bringing out language.
10. What do the first days of therapy look like?
You’ve probably caught on by now that services vary per provider. Everyone is usually nervous on the first day. I even get nervous on the first day because I’m meeting someone new and I hope the person likes me. To prepare ourselves, ask if you’ll be involved in the first session or if you just drop off your child. Some providers will meet with you to discuss policy and procedures and answer any questions about your child’s programs. If dropping off at a clinic, be sure to ask what to bring, such as a change of clothes, snacks, etc.
Regarding your child’s first sessions, therapy will be light and playful because therapists are building rapport with your child. Once they have gotten to know each other and built trust, then the therapist will slowly add in demands and target goals. This can take anywhere from a day to a week depending on how your child adjusts to therapy. After that, your child should be working on all of their goals written in the behavior plan.
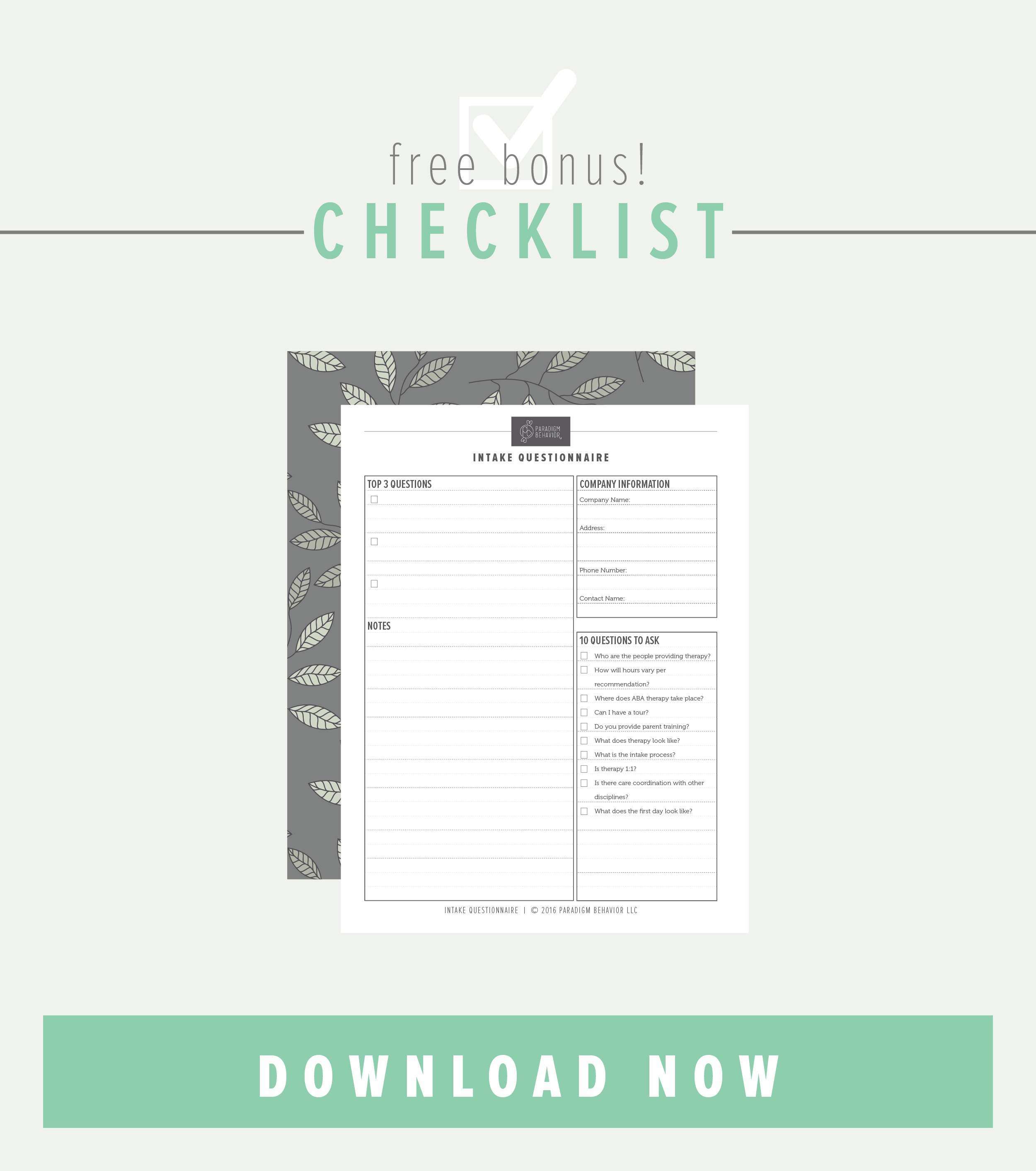
There’s a lot to take in and you may still have some other questions, but write them down! Hopefully, this provides you with a little insight on what to expect when starting ABA services. To help you find a provider that best suits your needs, I’ve created a handy dandy checklist of these top 10 questions along with organizational notes for your search. Subscribe to our free resource library to download the checklist. Want to learn more about ABA? As a bonus you'll also receive a free copy of our What is ABA? parent guide in your welcome email.